What is COPD?
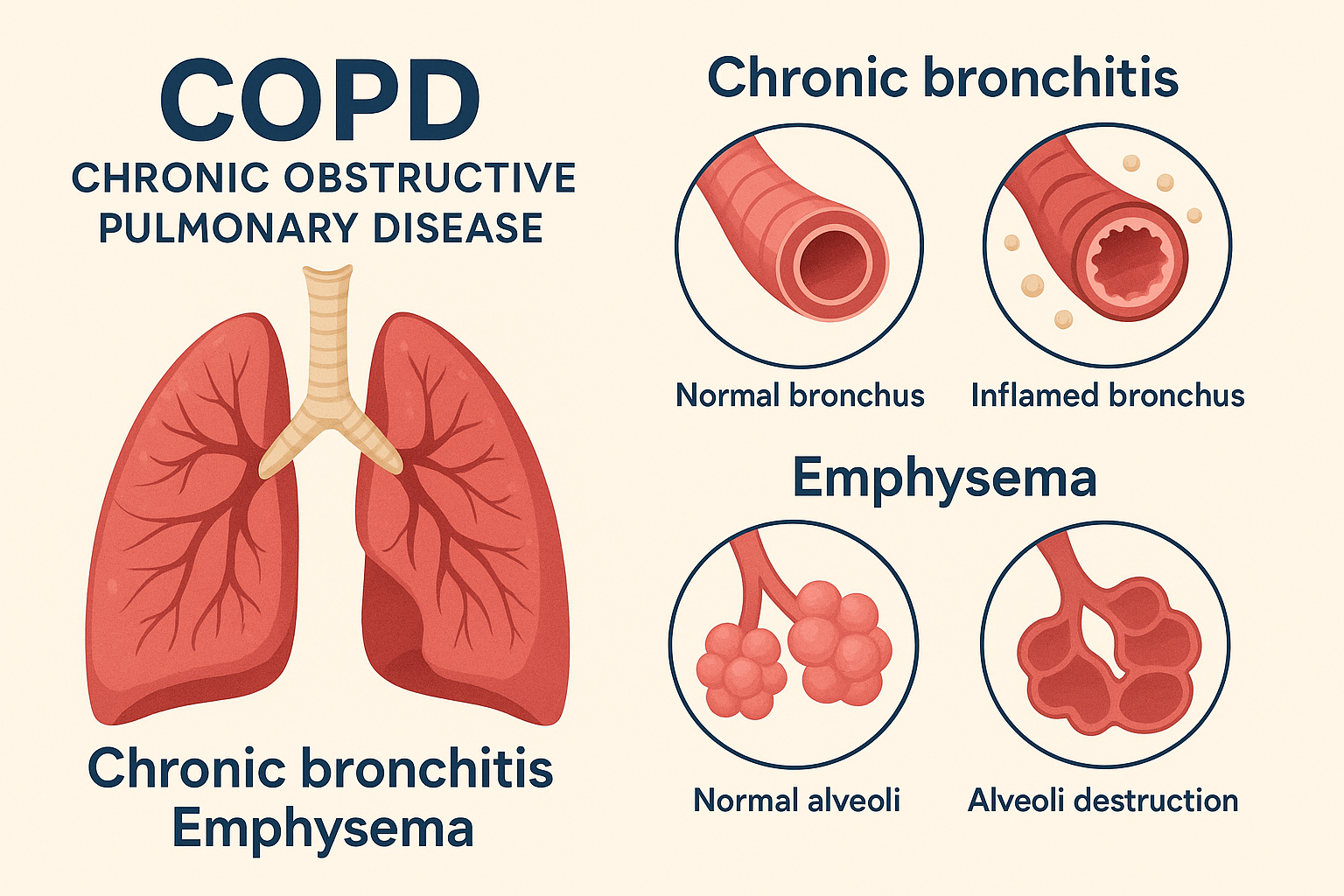
COPD is an umbrella term for a group of progressive lung diseases, including chronic bronchitis and emphysema, that cause airflow blockage and breathing-related problems. Most cases are caused by long-term exposure to irritants like cigarette smoke, air pollution, or occupational dust.
Key symptoms include:
- Chronic cough
- Shortness of breath
- Wheezing
- Fatigue
- Frequent respiratory infections
COPD is typically diagnosed through spirometry testing, which measures lung function.
Goals of COPD therapy
Though COPD can’t be reversed, treatments aim to:
- Relieve symptoms
- Prevent exacerbations (flare-ups)
- Improve quality of life
- Slow progression
- Reduce hospital admissions
Treatment is often personalized and may involve a combination of medications, lifestyle changes, and therapies.
Medication options
1. Bronchodilators
These are inhaled drugs that help relax airway muscles and improve airflow. They come in short-acting (e.g., albuterol) for quick relief and long-acting (e.g., tiotropium, salmeterol) for maintenance.
2. Inhaled corticosteroids
Used to reduce inflammation in the lungs and prevent exacerbations, especially in patients with frequent flare-ups.
3. Combination inhalers
Medications that combine bronchodilators and corticosteroids (e.g., Advair, Symbicort) offer convenience and broader symptom control.
4. Phosphodiesterase-4 inhibitors
Roflumilast may be prescribed for patients with chronic bronchitis to reduce inflammation.
5. Antibiotics and antivirals
Used during exacerbations triggered by infections.
Pulmonary rehabilitation: a powerful therapy
One of the most effective non-drug treatments for COPD is pulmonary rehabilitation — a supervised program that includes:
- Exercise training
- Nutritional counseling
- Education on lung health
- Psychological support
Pulmonary rehab improves endurance, reduces symptoms, and helps patients maintain independence. Many studies show it can significantly improve quality of life and reduce hospital visits.
Oxygen therapy
If blood oxygen levels are consistently low, supplemental oxygen may be prescribed. This can be delivered via:
- Nasal cannula
- Oxygen tanks or concentrators (portable or stationary)
- Non-invasive ventilation devices (e.g., BiPAP)
Oxygen therapy doesn’t treat COPD itself, but it helps prevent complications from low oxygen, such as heart strain or confusion.
Lifestyle modifications and self-management
Effective COPD management requires daily attention. Key strategies include:
- Smoking cessation – The single most important step for smokers
- Vaccinations – Yearly flu and pneumonia vaccines reduce infection risks
- Healthy diet and hydration – To maintain energy and immune function
- Breathing techniques – Such as pursed-lip breathing and diaphragmatic breathing
- Avoiding triggers – Including cold air, pollution, and dust
Patient education plays a critical role. The more informed you are, the more empowered you become.
Surgical options (in advanced cases)
For patients with severe COPD, especially emphysema, surgery may be considered:
- Lung volume reduction surgery (LVRS) – Removes damaged lung tissue to improve function
- Bullectomy – Removes large air sacs (bullae) that interfere with breathing
- Lung transplant – Considered in select patients under age 65 with very advanced disease
These are last-resort options, typically after all other treatments have been exhausted.
Looking ahead: life with COPD
Living with COPD is not easy — it’s a condition that demands daily attention, lifestyle changes, and emotional resilience. But thanks to modern medicine, personalized therapy, and patient education, many people are living longer, fuller lives despite the diagnosis.
The key lies in early intervention and ongoing support. When patients and caregivers work closely with healthcare teams, stay informed, and take an active role in managing symptoms, the outcome can be significantly better than expected.
COPD is a chronic illness, but it is not the end of independence, purpose, or joy. Each small step — from using an inhaler correctly to attending pulmonary rehab — adds up to a stronger, more empowered approach to living.
Considering the future
As COPD progresses, some patients may find themselves facing difficult decisions about care, especially when traditional therapies stop working. It’s during these moments that people may begin to wonder — what comes next?
At Tomorrow.bio, we provide information about an emerging option called human cryopreservation. This process involves preserving individuals at ultra-low temperatures after legal death, with the hope that future science might one day make revival and treatment possible.
It’s not a guaranteed solution. It’s not a replacement for palliative care or hospice. But it is an opportunity to preserve life when current medicine can go no further. And for some, that possibility is meaningful. We’re here to offer honest answers, not promises — and to walk with you if you're curious about what lies beyond the limits of today.
About Tomorrow.bio
At Tomorrow.bio, we are dedicated to advancing the science of cryopreservation with the goal of giving people a second chance at life. As Europe’s leading human cryopreservation provider, we focus on rapid, high-quality standby, stabilization, and storage of terminal patients — preserving them until future medical technologies may allow revival and treatment.
Our mission is to make human cryopreservation a reliable and accessible option for everyone. We believe that no life should end because current medical capabilities fall short.
Our vision is a future where death is optional — where people have the freedom to choose long-term preservation in the face of terminal illness or fatal injury, and to awaken when medicine has caught up.
📧 Contact us at: hello@tomorrow.bio
🌐 Visit our website: www.tomorrow.bio
🤝 Schedule a call with our team: Book a call



