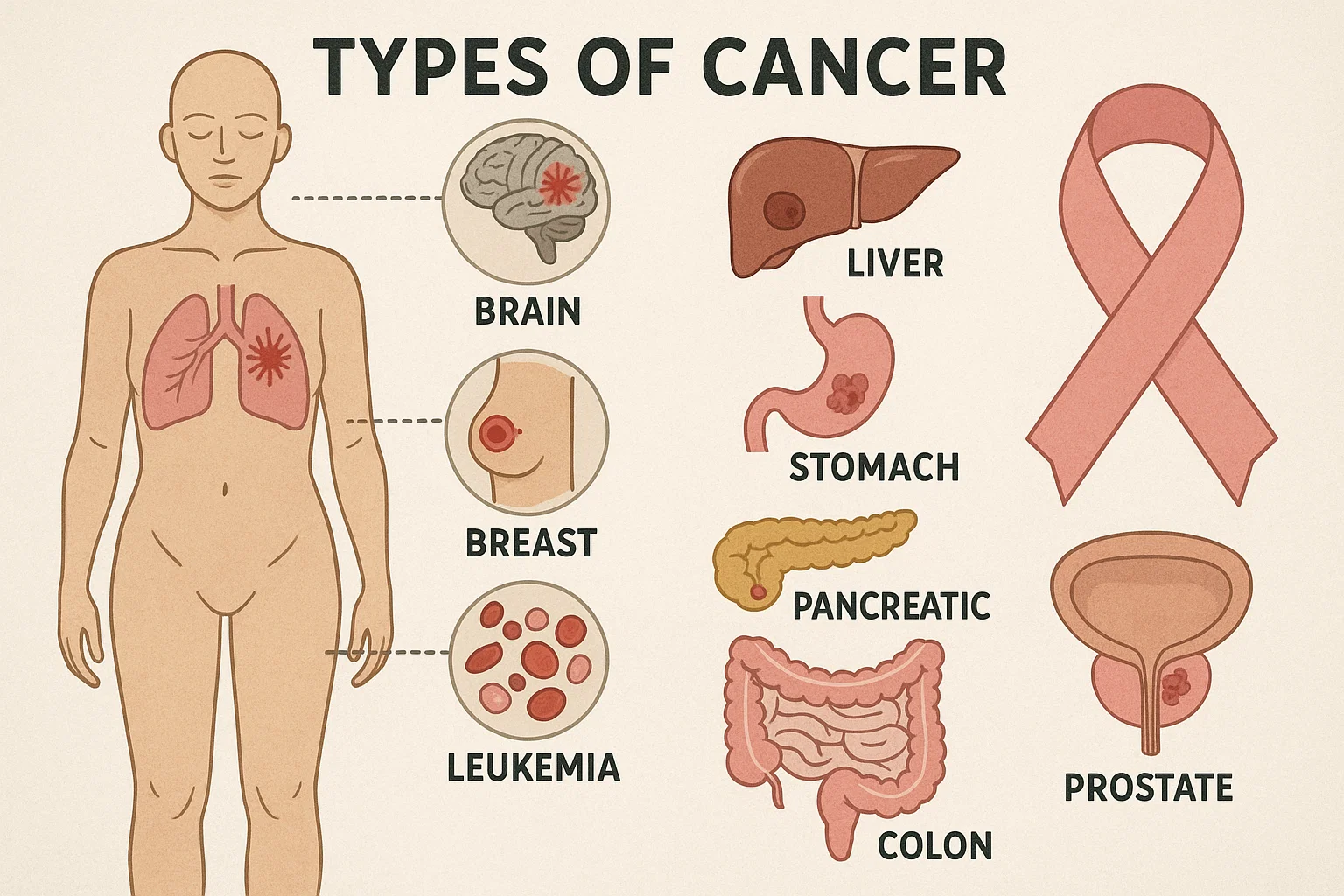
Although cancer encompasses over 200 distinct disorders, they share a common thread: uncontrolled cell growth. Classifying these diseases into coherent categories helps clarify diagnosis, guide therapies and set realistic expectations. In this article, we explore each major type in depth, citing cutting-edge research and linking to related insights on prognosis and underlying factors.
Carcinomas: Tumors of epithelial origin
Carcinomas arise from epithelial cells lining organs and vessels, accounting for approximately 80 percent of adult diagnoses. Key subtypes include:
- Adenocarcinoma: Originates in glandular tissue of the lungs, colon, prostate or pancreas. Early-stage lung adenocarcinoma often remains asymptomatic, underscoring the importance of low-dose CT screening in high-risk individuals
- Squamous cell carcinoma: Develops in skin, oral cavity, esophagus and cervix. Chronic irritation, such as tobacco exposure in the esophagus, elevates risk. For an overview of prognosis after esophageal adenocarcinoma diagnosis, see our analysis of esophageal cancer outcomes i
Carcinomas generally spread via lymphatics, leading to nodal involvement. Surgical resection remains the cornerstone for localized disease, while systemic therapies, hormone blockers in breast adenocarcinoma or targeted inhibitors in prostate cancer, are key for advanced cases.
Sarcomas: Connective tissue malignancies
Sarcomas originate in mesenchymal tissues, bone, cartilage, fat, muscle and vessels, and comprise 1 percent of adult cases but a higher share in children. Main categories:
- Osteosarcoma: The most common bone sarcoma in adolescents. Rapid bone turnover and active growth plates may predispose to genetic mutations in osteoblasts.
- Liposarcoma: Arises in adipocytes, often in deep soft-tissue compartments. Complete surgical excision with clear margins is critical; recurrence risk remains high without adjuvant radiotherapy.
- Leiomyosarcoma: Develops in smooth muscle, frequently in the uterus or retroperitoneum. Tumor size and mitotic index guide prognosis.
Unlike carcinomas, sarcomas less commonly involve lymph nodes but can metastasize hematogenously to the lungs or liver. Multimodal management—combining surgery, radiation and chemotherapy, is tailored by histologic grade and anatomic location.
Hematologic Cancers: Leukemias and lymphomas
Blood-forming tissues give rise to two major groups:
- Leukemia: Malignancy of bone-marrow progenitors, subdivided into acute versus chronic, and myeloid versus lymphoid.
- Acute myeloid leukemia (AML) features rapid proliferation of myeloblasts, requiring prompt induction regimens.
- Chronic lymphocytic leukemia (CLL) often follows an indolent course but can transform into aggressive lymphoma.
- Lymphoma: Neoplasms of lymphocytes, categorized as Hodgkin or non-Hodgkin.
- Diffuse large B-cell lymphoma (DLBCL) is the most common aggressive subtype, treated with immunochemotherapy (e.g., R-CHOP).
- Follicular lymphoma tends to grow slowly; “watch and wait” may be employed until symptomatic.
Hematologic cancers uniquely allow for transplantation of healthy stem cells to reconstitute marrow, a strategy not available for solid tumors. Survival varies widely by subtype and stage, with five-year rates exceeding 90 percent in early-stage Hodgkin lymphoma.
Central nervous system tumors
Primary brain and spinal cord tumors range from benign meningiomas to highly aggressive glioblastoma. Factors to consider:
- Glioblastoma multiforme (GBM): Characterized by diffuse infiltration and rapid recurrence. Its average survival remains under 18 months despite maximal resection, radiotherapy and temozolomide.
- Meningioma: Often benign and slow-growing, arising from the arachnoid layer. Surgical removal may be curative, but location near critical structures complicates intervention.
- Medulloblastoma: A pediatric embryonal tumor in the cerebellum, now classified by molecular subgroup, which refines risk stratification and treatment intensity.
Blood–brain barrier permeability limits systemic therapy efficacy, making surgical and radiotherapeutic advances essential. For those facing late-stage central nervous system disease, considering future-oriented options may offer additional hope.
Skin Cancers: Melanoma and non-melanoma
Cutaneous malignancies are the most visible yet diverse:
- Basal cell carcinoma (BCC): Slow-growing and locally invasive, rarely metastasizing; treated effectively with Mohs surgery.
- Squamous cell carcinoma (SCC): Greater metastatic potential than BCC, especially in immunocompromised hosts.
- Melanoma: The most aggressive form, arising from melanocytes. Early-detection via the “ABCDE” criteria (asymmetry, border irregularity, color variation, diameter and evolution) is lifesaving. Advanced melanoma now benefits from immunotherapy (checkpoint inhibitors) and targeted BRAF/MEK inhibitors.
Dermatoscopic screening and public awareness campaigns have improved early diagnosis, dramatically increasing cure rates for thin melanomas.
Rare & pediatric cancers
While each type is uncommon, collectively they represent a significant burden:
- Neuroblastoma in infants arises from adrenergic precursors, with outcomes linked to MYCN amplification status.
- Ewing sarcoma strikes adolescents’ bones and soft tissue, treated with multimodal regimens including chemotherapy, surgery and radiation.
- Retinoblastoma: an eye tumor in young children, now sees excellent survival with enucleation or focal therapies when detected early.
Clinical trials and international consortia drive progress, but rarity poses challenges for data collection and standardization.
When treatment options are exhausted
Facing a terminal diagnosis is profoundly difficult. Standard therapies focus on symptom relief and quality of life. Yet for patients and families seeking additional avenues, cryopreservation offers a future-facing opportunity. While not a cure, it preserves tissues at ultra-low temperatures until novel therapies—perhaps targeting minimal residual disease at the molecular level, become viable.
Understanding the unique biology, spread patterns and treatment pathways of each cancer type empowers informed decision-making. While current therapies offer remission or control in many cases, technology limitations still leave some with few options. Cryopreservation is not a cure but an opportunity to extend hope, serving as a bridge to tomorrow’s breakthroughs.
About Tomorrow.bio
At Tomorrow.bio we are dedicated to advancing the science of cryopreservation with the goal of giving people a second chance at life As Europe’s leading human cryopreservation provider we focus on rapid high-quality standby, stabilization and storage of terminal patients preserving them until future technologies may allow revival and treatment.
Our mission is to make human cryopreservation a reliable and accessible option for everyone We believe that no life should end because current capabilities fall short.
Our vision is a future where death is optional where people have the freedom to choose long-term preservation in the face of terminal illness or fatal injury and to awaken when science has caught upInterested in learning more or becoming a member
📧 Contact us at hello@tomorrow.bio
🌐 Visit our website www.tomorrow.bio
🤝 Schedule a call with our team Book a consultation



